Diabetic Foot Conditions
What Does Diabetes Do to Your Feet?
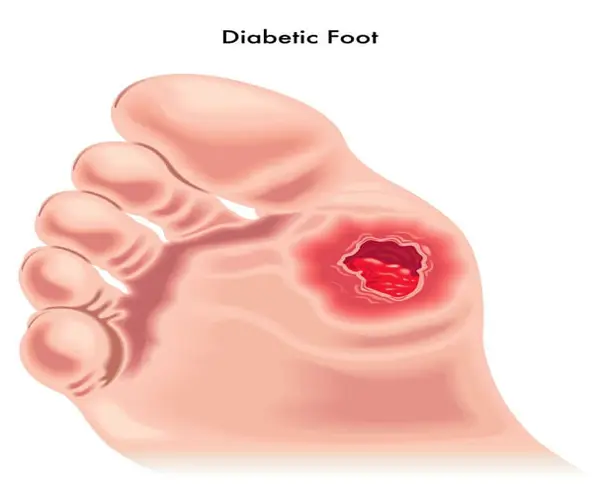
Diabetes, when unmanaged, can have serious effects on your feet. Dr. Ryan M. Sherick, a renowned expert in Los Angeles and Thousand Oaks, California emphasizes that high blood sugar levels can damage nerves and blood vessels, leading to diabetic neuropathy and poor circulation in the feet. This can result in reduced sensation, making it difficult to detect injuries and infections. Furthermore, impaired blood flow can slow down the healing process, increasing the risk of ulcers and even amputations.
Dr. Sherick advises diligent foot care, including daily inspections, proper footwear, and regular check-ups, to mitigate these risks and maintain good foot health for those living with diabetes

Why do diabetics have foot problems?
Diabetics often experience foot problems due to a condition called diabetic neuropathy. This condition occurs when high levels of glucose in the blood damage the nerves over time. As a result, diabetics may lose sensation in their feet or experience altered sensations like tingling and numbness. This loss of feeling can lead to several issues.
For diabetics, it’s crucial to maintain strict blood sugar control, inspect their feet regularly, and seek prompt medical attention for any foot issues to prevent or manage these complications.
What is diabetic peripheral neuropathy?
Diabetic peripheral neuropathy (DPN) is a common complication of diabetes. It results from prolonged high blood sugar levels damaging nerves, especially in the legs and feet. DPN can cause numbness, tingling, and pain in these areas. Over time, it may lead to loss of sensation and muscle weakness, making injuries harder to detect. Proper diabetes management, including blood sugar control and lifestyle changes, can help prevent or slow the progression of DPN. Regular check-ups with a healthcare provider are essential for early detection and management of this condition.
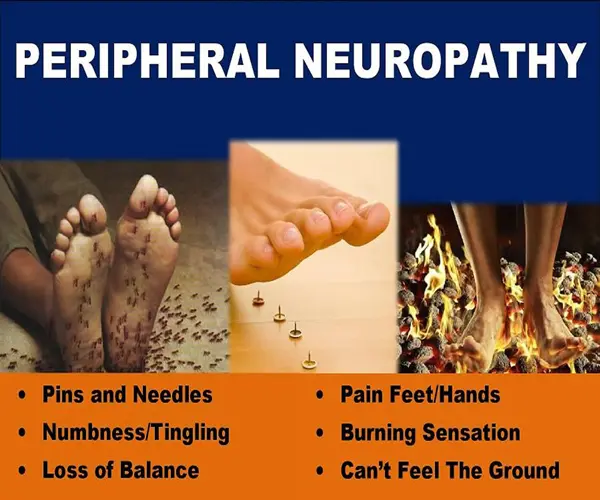
What does neuropathy feel like?
The first signs of diabetic peripheral neuropathy are when you start to feel numbness and tingling in your body.
When your blood sugar is too high, it not only harms your nerve cells but also makes them take in more water. This swelling of nerve cells puts pressure on the nerves themselves. Medical experts haven’t figured out how to stop diabetic neuropathy from happening, but there are ways to slow it down or even stop it from getting worse. To do this, they relieve the pressure that affects both the nerves and blood vessels.
If they do this pressure-relief surgery early on in diabetic neuropathy, it can help restore blood flow. This will make the numbness and tingling go away and let your nerves heal.
What is peripheral vascular disease (PVD)?
Peripheral Vascular Disease (PVD) is a condition that affects blood vessels outside the heart and brain. It typically involves narrowing or blockage of arteries in the legs, reducing blood flow. Symptoms may include pain, cramping, and numbness in the limbs. PVD is often linked to atherosclerosis and can increase the risk of serious health issues if left untreated.
Neuropathy and PVD can cause the
following foot problems for diabetics:
Neuropathy and Peripheral Vascular Disease (PVD) are two common complications that affect many individuals with diabetes, and when combined, they can lead to a host of foot problems. These issues are of particular concern because they can result in severe consequences, including amputation, if not properly managed. Here, we will discuss the foot problems that diabetics may experience when dealing with neuropathy and PVD.
How to take care of your diabetic feet?
Taking care of your diabetic feet is crucial to maintain good health and prevent serious complications. Diabetes can lead to poor blood circulation and nerve damage, making the feet vulnerable to infections and slow-healing wounds. Here are some essential tips to keep your feet healthy:
Taking care of your diabetic feet is a lifelong commitment that can significantly reduce the risk of serious complications and Dr. Ryan M. Sherick can be a valuable person to help you do so. By following these guidelines, you can help ensure your feet remain healthy and pain-free, allowing you to lead an active and fulfilling life despite diabetes.
When to see a doctor about your diabetic foot problems?
If you have type 1 or type 2 diabetes, you should already be visiting your doctor regularly. But if you see any of the following changes or experience new symptoms, it’s important to seek medical help:
Why choose Apex Foot & Ankle Institute for diabetic foot care?
When it comes to diabetic foot care in Los Angeles or Thousand Oaks, California there’s no better choice than Apex Foot & Ankle Institute, led by Dr. Ryan M. Sherick.
Here’s why you should entrust your diabetic foot health to our expert team:
Your feet deserve the best care. Choose Apex Foot & Ankle Institute in Thousand Oaks, California and the Los Angeles area for top-notch diabetic foot care that prioritizes your health and well-being.
Request An Appointment
Need Help With Your Foot And Ankle?
