Foot & Ankle Cartilage Repair
Cartilage Regeneration Benefits Thousand Oaks Athletes and Baby Boomers with Aching Ankles
Revolutionary cartilage regeneration isn’t a magical fountain of youth, but it comes pretty close for older folks and athletes with painful ankle joints. It can make them feel almost as good as new, especially with new innovative cartilage regeneration techniques used by Dr. Ryan M. Sherick at the Apex Foot & Ankle Institute in Thousand Oaks, California.

New Innovative Cartilage Repair Options Now Available to patients in Conejo Valley, Westlake Village, and Thousand Oaks.
Learn more about the new and improved surgery techniques for foot and ankle cartilage repair and regeneration like bioengineered scaffolds for reconstructing joints, microfracture techniques, and stem cell cartilage regeneration. These techniques can create new cartilage-like structures where there were gaps before leaving patients.
These discoveries are good news. Lots of older folks, especially baby boomers, often have ankle issues because our joints wear out as we get older which many people attribute to arthritis of the foot and ankle. When joints become weaker, it’s easier to get hurt. For athletes, using their joints a lot or getting injured can damage the cartilage. In the past, losing cartilage meant losing the ability to use the joint properly. But now, with advanced techniques that Dr. Ryan M. Sherick has extensive experience using gives patients a new advantage unlike before with cartilage regeneration now possible.
Newer innovative surgical techniques for cartilage regeneration use special materials to support the body’s healing process. They help the body create new cartilage and fix torn ligaments and joints. Some of these procedures can even be done in a doctor’s office.
Dr. Ryan M. Sherick, who is a Fellowship-trained and board-certified Foot and Ankle Surgeon, who is sharing his knowledge to make these treatments better. He’s worked a lot with athletes, so he knows what their bodies need.
Dr. Sherick says, “Treating athletes requires knowing a lot about the sports they play. New methods for fixing joint damage can get our athletes back to their sports faster and, in some cases, keep them playing for longer.”
These advancements in cartilage regeneration help all patients get back to their normal lives faster than ever before. It’s not like turning back time or erasing our mistakes, but most patients agree it’s pretty close.
Dr. Sherick is a leader in using the latest technology to treat cartilage problems in the lower part of the body. He is often found teaching and speaking nationally to other foot and ankle surgeons about these advanced methods during training labs.
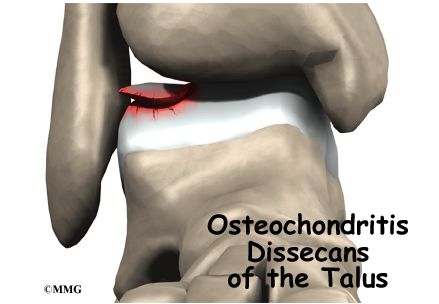
Talar Dome Lesion
A talar dome lesion is a condition that affects the cartilage and bone of the talus, which is one of the major bones in the human foot and plays a crucial role in ankle movement. In this article, we will explore what a talar dome lesion is, its signs and symptoms, diagnosis, nonsurgical treatment approaches, the indications for surgery, potential complications, and introduce Dr. Ryan M. Sherick, a medical professional specializing in this field.
What Is a Talar Dome Lesion?
A talar dome lesion, often referred to as osteochondral lesion of the talus (OLT), is a condition characterized by damage or degeneration of the cartilage and underlying bone in the talus. This can result from traumatic injuries, such as ankle sprains or fractures, or may develop over time due to repetitive stress on the ankle joint. The talar dome is a crucial part of the ankle joint, as it bears much of the body’s weight during activities like walking, running, and jumping.
Signs & Symptoms
Patients with talar dome lesions often experience symptoms such as:
The severity of these symptoms can vary, with some individuals experiencing occasional discomfort while others endure persistent pain and impaired mobility.
Diagnosis
Diagnosing a talar dome lesion typically involves a thorough examination by a medical professional like Dr. Ryan M. Sherick, who specializes in orthopedics and foot and ankle disorders. Diagnostic methods include:
Nonsurgical Treatment Approaches
Nonsurgical treatment options are often considered as the initial approach to manage talar dome lesions. These may include:
Dr. Ryan M. Sherick may recommend a combination of these treatments tailored to the individual’s condition and lifestyle.
When Is Surgery Needed for Ankle or Foot Cartilage damage?
Surgery becomes necessary when conservative treatments do not provide sufficient relief or when the lesion is severe. Surgical procedures to address talar dome lesions may include:
The decision for surgery and the specific technique used depend on the patient’s condition and the recommendation of a skilled orthopedic surgeon like Dr. Ryan M. Sherick.
Complications of Talar Dome Lesions
Left untreated or inadequately managed, talar dome lesions can lead to several complications, including:
To prevent these complications, early diagnosis and appropriate treatment are essential.
Dr. Ryan M. Sherick is a renowned foot and ankle specialist with extensive experience in treating talar dome lesions and a wide range of foot and ankle conditions. His expertise, combined with a patient-centered approach, ensures that individuals with talar dome lesions receive the most effective and tailored care for their condition.
Talar dome lesions can cause significant pain and discomfort, but with the right diagnosis and treatment approach, patients can regain their mobility and enjoy an improved quality of life. Dr. Ryan M. Sherick in Thousand Oaks, California is well-equipped to provide the best care and guidance for individuals suffering from this condition.
Conservative Treatment of Ankle Cartilage and Foot Cartilage Damage in addition to Ankle Osteoarthritis
Can Platelet-Rich Plasma Effectively Postpone Surgery?
Cartilage injuries in the foot and ankle or specifically Ankle osteoarthritis can be a debilitating condition, causing pain and limited mobility. For many patients, surgery seems like the only option. However, there is growing interest in conservative treatments that may postpone or even eliminate the need for surgery. Platelet-rich plasma (PRP) therapy is one such option.
PRP involves drawing a small sample of the patient’s blood, processing it to concentrate the platelets, growth factors, and other healing components, and then injecting it into the affected joint. Studies suggest that PRP may help reduce pain and inflammation, stimulate tissue regeneration, and improve joint function in ankle osteoarthritis.
While research is ongoing, PRP has shown promise in providing relief for some patients, potentially delaying the need for surgery. However, the effectiveness of PRP can vary from person to person, and it may not be a suitable treatment for everyone. Consult with a healthcare professional to determine if PRP is a viable option for managing ankle osteoarthritis and postponing surgery.

What is BioCartilage?
BioCartilage is a cutting-edge, regenerative tissue implant used in orthopedic and sports medicine. It is a bioinductive scaffold designed to repair damaged cartilage in joints, particularly the knee. BioCartilage contains a mixture of hyaluronic acid and fibers, creating a supportive matrix. When implanted in a damaged joint, it encourages the body’s natural healing processes, stimulating the growth of new, healthy cartilage. This innovative approach can alleviate pain, improve joint function, and delay or even eliminate the need for more invasive procedures like joint replacement surgery. BioCartilage represents a promising advancement in the field of regenerative medicine, offering hope for those with cartilage-related joint issues.

What are osteochondral defects?
Osteochondral defects, often referred to as cartilage lesions, are a type of joint disorder that affects the smooth, protective cartilage covering the ends of bones within a joint. These defects typically occur in weight-bearing joints such as the knee, ankle, or hip, and they can result from various causes, including trauma, repetitive stress, genetic predisposition, or degenerative conditions.
The main characteristic of osteochondral defects is damage to both the cartilage and the underlying bone. This can lead to pain, swelling, and decreased joint function. In the early stages, patients may experience discomfort and stiffness during physical activity, which can progress to chronic pain and limited mobility if left untreated. Osteochondral defects are diagnosed through imaging techniques like X-rays, MRI, or arthroscopy.
Treatment options for osteochondral defects vary based on the size, location, and severity of the lesion. They range from non-surgical interventions like physical therapy and anti-inflammatory medications to surgical procedures such as microfracture, osteochondral autograft or allograft transplantation, or autologous chondrocyte implantation. Timely diagnosis and appropriate treatment are crucial to prevent further joint deterioration and maintain a good quality of life for individuals affected by these defects.
How do cartilage transplants improve osteochondral lesion treatment?
Cartilage transplants offer a promising avenue for improving the treatment of osteochondral lesions, which involve damage to both cartilage and underlying bone in weight-bearing joints. These lesions are challenging to treat because of the limited regenerative capacity of cartilage. Cartilage transplants, however, provide a solution by replacing damaged tissue with healthy cartilage, facilitating the restoration of joint function and reducing pain.
Autograft transplantation involves using a patient’s own cartilage from a less weight-bearing area, while allograft transplantation utilizes donor cartilage. Autografts ensure compatibility but might create additional joint trauma. Allografts are a viable option when large defects need repair. In some cases, autologous chondrocyte implantation (ACI) is used, where a patient’s own cartilage cells are harvested, cultured, and then implanted in the lesion site.
These techniques improve treatment outcomes by promoting cartilage repair and preventing further joint degeneration. While not suitable for all cases, cartilage transplants represent a valuable tool in the orthopedic arsenal for managing osteochondral lesions and helping patients regain mobility and reduce pain.
Recovery from Osteochondral lesion repair with BioCartilage
Recovery from osteochondral lesion repair with BioCartilage is a progressive journey. After the procedure, patients typically undergo a period of rest and limited weight-bearing. Physical therapy plays a crucial role in the rehabilitation process, helping to regain joint strength and mobility. Over time, the BioCartilage stimulates the growth of healthy cartilage, improving joint function and reducing pain. The full recovery timeline can vary based on the lesion’s size and location, but BioCartilage offers a promising path to long-term joint health, often enabling individuals to return to their active lifestyles with improved joint function and reduced discomfort.
Apex Foot and Ankle Institute, the right choice
Apex Foot and Ankle Institute is the ideal choice for comprehensive foot and ankle care. With a team of experienced podiatrists, cutting-edge technology, and a patient-centered approach, we provide top-notch diagnostic, treatment, and surgical services. Whether you’re dealing with common issues like bunions and plantar fasciitis or complex conditions, we offer tailored solutions for all your foot and ankle needs. Your comfort and well-being are our priorities, making Apex Foot and Ankle Institute the right choice for your podiatric care, ensuring you get back on your feet with confidence.
DeNovo Cartilage Repair
DeNovo cartilage repair is a cutting-edge medical approach for treating damaged or deteriorating cartilage in joints. This innovative technique focuses on regenerating cartilage tissue without the need for invasive surgeries like joint replacements. DeNovo involves the transplantation of juvenile cartilage cells into the affected area, promoting natural healing and reducing pain, stiffness, and discomfort.

One of the key advantages of DeNovo cartilage repair is its minimally invasive nature. It offers patients a quicker recovery time, allowing them to return to their normal activities sooner. Additionally, this procedure has shown promising results in promoting long-term joint health and function, making it a potential game-changer in the field of orthopedic medicine.
While DeNovo cartilage repair is still a developing area of medicine, it holds great promise for individuals suffering from joint problems. As researchers continue to refine and expand upon this technique, it offers hope for a future where cartilage damage may be effectively treated with less invasive and more patient-friendly approaches.
Traditional Methods to Ankle Cartilage Replacement
Traditional methods for ankle cartilage replacement have long been relied upon to address cartilage damage and joint-related issues. One such method is microfracture surgery, which involves creating small holes in the affected area, stimulating the body’s natural healing process by releasing blood and stem cells. While this technique is less invasive, it may not provide long-lasting relief for more severe cartilage damage.
Another traditional approach is autologous chondrocyte implantation (ACI), where healthy cartilage cells are harvested from the patient’s own body, grown in a lab, and then transplanted into the damaged area. This method has demonstrated success in promoting cartilage regrowth and improving joint function, particularly for individuals with localized cartilage defects.
Osteochondral allograft transplantation is yet another traditional method that involves replacing damaged cartilage with donor tissue. This technique is effective for larger areas of cartilage damage and provides an immediate solution, although it may come with potential limitations such as donor tissue availability and compatibility. These time-tested approaches to ankle cartilage replacement offer viable options for patients seeking relief from cartilage-related ankle problems, each with its own set of advantages and considerations.
The DeNovo Cartilage Repair Technique
The DeNovo cartilage repair technique is a cutting-edge medical procedure designed to address cartilage damage in joints, particularly the knee. Unlike invasive surgeries, DeNovo involves the transplantation of juvenile cartilage cells, fostering natural healing. This minimally invasive method has the advantage of a shorter recovery time and a reduction in pain and stiffness, providing a promising solution for those suffering from cartilage-related joint issues. As this technique continues to evolve, it holds significant promise for enhancing the quality of life for individuals dealing with cartilage damage.
The Regenerative Advantage of DeNovo Cartilage Repair
DeNovo cartilage repair offers a regenerative advantage by harnessing the body’s natural healing capabilities. This innovative procedure involves the transplantation of juvenile cartilage cells, promoting the regeneration of damaged cartilage in joints. Unlike traditional methods, DeNovo encourages the body to heal itself, minimizing the need for invasive surgery. This approach not only reduces pain and discomfort but also results in a quicker recovery. By leveraging the body’s innate regenerative potential, DeNovo cartilage repair stands at the forefront of orthopedic medicine, providing promising outcomes for those in need of effective and less invasive cartilage restoration solutions.
Request An Appointment
Need Help With Your Foot And Ankle?
